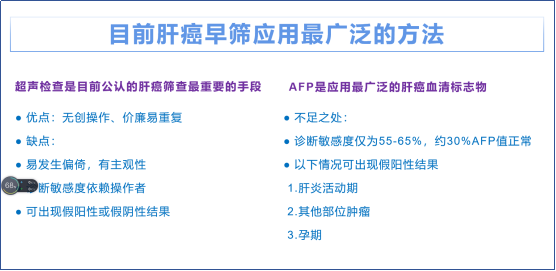
肝内胆管癌的诊治新进展 肝内胆管癌(ICC)是原发性肝癌的一种,近年来发病率和病死率均呈上升趋势,患者预后极差。目前ICC的临床诊治面临检出率低、病死率高、治疗预后差的难题,亟须深入研究以促进临床诊治水平的提高。近年来,ICC诊治相关的研究在很多方面取得了新的进展,我们应及时更新关于ICC临床诊治新进展的知识。本文回顾了近几年的ICC方面的最新研究成果,总结关于ICC分型、预防及诊断分期的新观点,以及在外科治疗、系统治疗方面取得的新进展,并探讨ICC个体化精准治疗的潜力及联合治疗导致罕见并发症发生的问题。
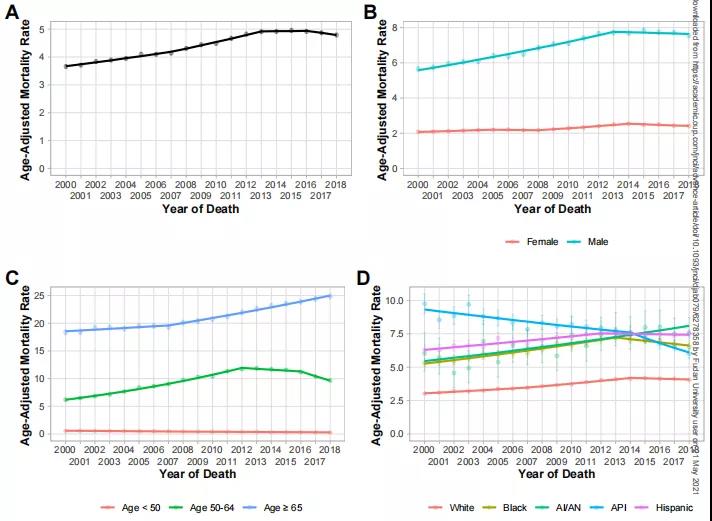
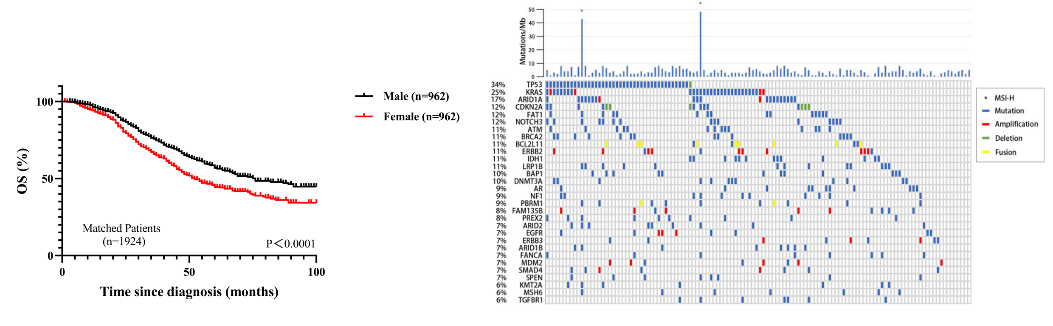
肝内胆管癌(intrahepatic cholangiocarcinoma,ICC)是起源自肝内胆管上皮细胞的一种原发性肝癌,其发病隐匿,早期临床症状不明显,且病情进展迅速,很多患者确诊时已处于晚期,预后往往很差[1]。根据美国国家卫生统计中心数据库的数据,ICC的5年总体生存率仅9%左右[2]。R0切除是唯一有可能根治ICC的治疗方法,但患者极易错过最佳的手术治疗时间窗。在深入理解ICC生物学特性的基础上,不断提高诊断的准确率和完善个体化的综合治疗方案,是解决ICC检出率低、病死率高、治疗预后差的关键。我们回顾了近年来ICC相关的最新研究成果,总结其临床诊治方面取得的进展,并探讨未来的临床实践方向及进一步研究应注意的问题,以期帮助临床医师更好地认识ICC的生物学特性,更新关于ICC临床诊治的知识。
一、ICC分型、预防及诊断分期的新观点
二、ICC的外科治疗新进展
三、ICC系统治疗的新进展
四、思考与展望
参考文献
[1]BanalesJM, MarinJ, LamarcaA, et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management[J].Nat Rev Gastroenterol Hepatol,2020,17(9):557-588. DOI: 10.1038/s41575-020-0310-z.
[2]YaoKJ, JabbourS,ParekhN, et al. Increasing mortality in the United States from cholangiocarcinoma: an analysis of the National Center for Health Statistics Database[J].BMC Gastroenterol,2016,16(1):117. DOI: 10.1186/s12876-016-0527-z.
[3]SakamotoY, KokudoN,MatsuyamaY, et al. Proposal of a new staging system for intrahepatic cholangiocarcinoma: Analysis of surgical patients from a nationwide survey of the Liver Cancer Study Group of Japan[J].Cancer,2016,122(1): 61-70. DOI: 10.1002/cncr.29686.
[4]中国抗癌协会肝癌专业委员会胆管癌协作组. 原发性肝癌诊疗指南之肝内胆管癌诊疗中国专家共识(2022版)[J]. 中华消化外科杂志, 2022,21(10):1269-1301. DOI: 10.3760/cma.j.cn115610-20220829-00476.
[5]EASL-ILCA Clinical Practice Guidelines on the management of intrahepatic cholangiocarcinoma[J].J Hepatol,2023,79(1):181-208. DOI: 10.1016/j.jhep.2023.03.010.
[6]YoonJG, KimMH, JangM, et al. Molecular Characterization of Biliary Tract Cancer Predicts Chemotherapy and Programmed Death 1/Programmed Death-Ligand 1 Blockade Responses[J]. Hepatology, 2021,74(4):1914-1931. DOI: 10.1002/hep.31862.
[7]AhnKS,O′BrienD,KangYN, et al. Prognostic subclass of intrahepatic cholangiocarcinoma by integrative molecular-clinical analysis and potential targeted approach[J].Hepatol Int,2019,13(4):490-500. DOI: 10.1007/s12072-019-09954-3.
[8]MaB, MengH, TianY, et al. Distinct clinical and prognostic implication of IDH1/2 mutation and other most frequent mutations in large duct and small duct subtypes of intrahepatic cholangiocarcinoma[J].BMC Cancer,2020,20(1):318. DOI: 10.1186/s12885-020-06804-6.
[9]ZhuAX, MacarullaT, JavleMM, et al. Final Overall Survival Efficacy Results of Ivosidenib for Patients With Advanced Cholangiocarcinoma With IDH1 Mutation: The Phase 3 Randomized Clinical ClarIDHy Trial[J].JAMA Oncol,2021,7(11):1669-1677. DOI:10.1001/jamaoncol.2021.3836.
[10]VogelA, SegattoO, StenzingerA, et al. FGFR2 Inhibition in Cholangiocarcinoma[J].Annu Rev Med, 2023, 74: 293-306. DOI: 10.1146/annurev-med-042921-024707.
[11]MoseleF, RemonJ, MateoJ, et al. Recommendations for the use of next-generation sequencing (NGS) for patients with metastatic cancers: a report from the ESMO Precision Medicine Working Group[J].Ann Oncol,2020,31(11): 1491-1505. DOI: 10.1016/j.annonc.2020.07.014.
[12]Bekaii-SaabTS,BridgewaterJ,NormannoN. Practical considerations in screening for genetic alterations in cholangiocarcinoma[J].Ann Oncol,2021,32(9):1111- 1126. DOI: 10.1016/j.annonc.2021.04.012.
[13]Uson JuniorP,BoradMJ. Precision approaches for cholangiocarcinoma: progress in clinical trials and beyond[J].Expert Opin Investig Drugs, 2022, 31(1): 125-131. DOI: 10.1080/13543784.2022.2017882.
[14]VogelA, BridgewaterJ, EdelineJ, et al. Biliary tract cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up[J].Ann Oncol,2023,34(2):127-140. DOI: 10.1016/j.annonc.2022.10.506.
[15]AliAH, TabibianJH, Nasser-GhodsiN,et al. Surveillance for hepatobiliary cancers in patients with primary sclerosing cholangitis[J].Hepatology, 2018,67(6):2338- 2351. DOI: 10.1002/hep.29730.
[16]BergquistA,WeismüllerTJ,LevyC,et al. Impact on follow-up strategies in patients with primary sclerosing cholangitis[J].Liver Int,2023,43(1):127-138. DOI: 10.1111/liv.15286.
[17]TovoliF,GuerraP,IavaroneM,et al. Surveillance for Hepatocellular Carcinoma Also Improves Survival of Incidentally Detected Intrahepatic Cholangiocarcinoma Arisen in Liver Cirrhosis[J].Liver Cancer,2020,9(6):744-755. DOI: 10.1159/000509059.
[18]JesperD,HeynSG,SchellhaasB,et al. Effects of liver cirrhosis and patient condition on clinical outcomes in intrahepatic cholangiocarcinoma: a RETrospective analysis of 156 cases in a single center[J].Eur J Gastroenterol Hepatol,2018,30(5):552-556. DOI:10.1097/MEG.0000000000001036.
[19]SiripongsakunS,VidhyarkornS,CharuswattanakulS,et al. UltRASound surveillance for cholangiocarcinoma in an endemic area: A prove of survival benefits[J]. J Gastroenterol Hepatol,2018,33(7):1383-1388. DOI: 10.1111/jgh.14074.
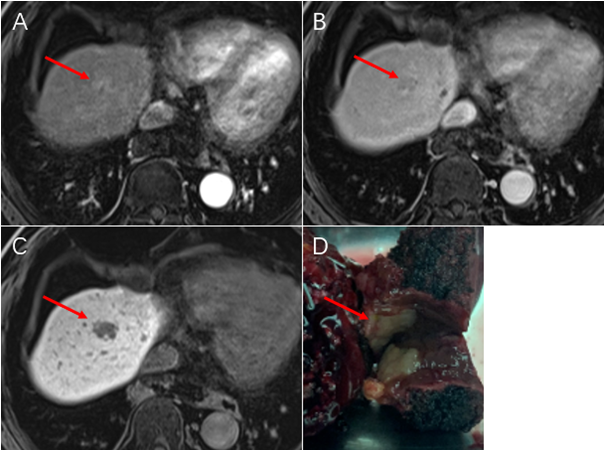
[20]KimYY,YeomSK,ShinH,et al. Clinical Staging of Mass-Forming Intrahepatic Cholangiocarcinoma: Computed Tomography Versus Magnetic Resonance Imaging[J].Hepatol Commun,2021,5(12):2009-2018. DOI: 10.1002/hep4.1774.
[21]JiangL,TanH,PanjeCM,et al. Role of 18F-FDG PET/CT imaging in intrahepatic cholangiocarcinoma[J].Clin Nucl Med,2016,41(1):1-7. DOI:10.1097/RLU.0000000000000998.
[22]LinY,ChongH,SongG,et al. The influence of (18)F-fluorodeoxyglucose positron emission tomography/computed tomography on the N-and M-staging and subsequent clinical management of intrahepatic cholangiocarcinoma[J].Hepatobiliary Surg Nutr,2022,11(5): 684-695. DOI: 10.21037/hbsn-21-25.
[23]SiA,LiJ,YangZ,et al. Impact of Anatomical Versus Non-anatomical Liver Resection on Short-and Long-Term Outcomes for Patients with Intrahepatic Cholangiocarcinoma[J].Ann Surg Oncol,2019,26(6):1841-1850. DOI: 10.1245/s10434-019-07260-8.
[24]韩祥松, 李全伟, 郭佩垒, 等. 两种肝切除方式对肝内胆管细胞性肝癌患者生存结局影响的多因素分析[J]. 中华医学杂志,2022,102(18):1364-1368. DOI: 10.3760/cma.j.cn112137-20220119-00142.
[25]de JongMC, NathanH, SotiropoulosGC, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment[J].J Clin Oncol,2011,29(23):3140-3145. DOI: 10.1200/JCO.2011.35.6519.
[26]BridgewaterJ,GallePR,KhanSA,et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma[J]. J Hepatol, 2014,60(6):1268-1289. DOI: 10.1016/j.jhep.2014.01.021.
[27]吴向嵩, 陈燕, 靳云鹏, 等. 解剖性肝切除在肝内胆管癌治疗中的价值[J].中华外科杂志, 2018, 56(4): 269-273. DOI: 10.3760/cma.j.issn.0529-5815.2018.04.005.
[28]LiuH, LinL, LinZ, et al. Impact of surgical margin width on long-term outcomes for intrahepatic cholangiocarcinoma: a multicenter study[J].BMC Cancer,2021, 21(1): 840. DOI: 10.1186/s12885-021-08560-7.
[29]DaiYS,HuHJ,LvTR,et al. The influence of resection margin width in patients with intrahepatic cholangiocarcinoma: a meta-analysis[J].World J Surg Oncol,2023,21(1):16. DOI:10.1186/s12957-023-02901-5.
[30]RuzzenenteA,ConciS,ViganòL,et al. Role of Lymph Node Dissection in Small (≤3 cm) Intrahepatic Cholangiocarcinoma[J].J Gastrointest Surg,2019,23(6):1122-1129. DOI: 10.1007/s11605-019-04108-0.
[31]BensonAB,D′AngelicaMI,AbbottDE,et al. Hepatobiliary Cancers, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology[J].J Natl Compr Canc Netw,2021,19(5): 541-565. DOI: 10.6004/jnccn.2021.0022.
[32]WeberSM,RiberoD,O′ReillyEM,et al. Intrahepatic cholangiocarcinoma: expert consensus statement[J].HPB (Oxford), 2015, 17(8): 669-680. DOI: 10.1111/hpb.12441.
[33]中国临床肿瘤学会指南工作委员会. 胆道恶性肿瘤诊疗指南2020[M]. 北京: 人民卫生出版社, 2020.
[34]ZhangXF,XueF,DongDH,et al. Number and station of lymph node metastasis after curative-intent resection of intrahepatic cholangiocarcinoma impact prognosis[J].Ann Surg,2021,274(6):e1187-e1195. DOI: 10.1097/SLA.0000000000003788.
[35]SpositoC,RattiF,CucchettiA,et al. Survival benefit of adequate lymphadenectomy in patients undergoing liver resection for clinically node-negative intrahepatic cholangiocarcinoma[J].J Hepatol,2023,78(2):356-363. DOI: 10.1016/j.jhep.2022.10.021.
[36]汤朝晖, 陈家璐, 刘深洋, 等. 靶免联合治疗在胆道恶性肿瘤转化中应用的意义[J].中华外科杂志,2022,60(4):343-350. DOI:10.3760/cma.j.cn112139-20220110-00019.
[37]Le RoyB,GelliM,PittauG,et al. Neoadjuvant chemotherapy for initially unresectable intrahepatic cholangiocarcinoma[J].Br J Surg,2018,105(7):839-847. DOI: 10.1002/bjs.10641.
[38]KamarajahS,GiovinazzoF,RobertsKJ,et al. The role of down staging treatment in the management of locally advanced intrahepatic cholangiocarcinoma: Review of literature and pooled analysis[J].Ann Hepatobiliary Pancreat Surg,2020,24(1):6-16. DOI: 10.14701/ahbps.2020.24.1.6.
[39]YadavS,XieH,Bin-RiazI,et al. Neoadjuvant vs. adjuvant chemotherapy for cholangiocarcinoma:a propensity score matched analysis[J].Eur J Surg Oncol,2019,45(8):1432-1438. DOI: 10.1016/j.ejso.2019.03.023.
[40]洪德飞,彭淑牖,刘允怡. ALPPS治疗肝细胞癌10年回望:永恒的理念 慎选的术式[J].中华外科杂志,2022,60(2):113-116. DOI:10.3760/cma.j.cn112139-20211021-00497.
[41]De MartinE,RayarM,GolseN,et al. Analysis of liver resection versus liver transplantation on outcome of small intrahepatic cholangiocarcinoma and combined hepatocellular-cholangiocarcinoma in the setting of cirrhosis[J].Liver Transpl,2020,26(6):785-798. DOI: 10.1002/lt.25737.
[42]SapisochinG,IvanicsT,HeimbachJ. Liver Transplantation for intrahepatic cholangiocarcinoma: ready for prime time?[J].Hepatology, 2022, 75(2): 455-472. DOI: 10.1002/hep.32258.
[43]SapisochinG,FacciutoM,Rubbia-BrandtL,et al. Liver transplantation for “very early” intrahepatic cholangiocarcinoma: International RETrospective study supporting a prospective assessment[J]. Hepatology, 2016, 64(4): 1178-1188. DOI: 10.1002/hep.28744.
[44]McMillanRR, JavleM,KodaliS,et al. Survival following liver transplantation for locally advanced, unresectable intrahepatic cholangiocarcinoma[J]. Am J Transplant,2022, 22(3): 823-832. DOI: 10.1111/ajt.16906.
[45]SapisochinG,JavleM,LerutJ,et al. Liver transplantation for cholangiocarcinoma and mixed hepatocellular cholangiocarcinoma: working group report from the ILTS Transplant Oncology Consensus Conference[J].Transplantation,2020,104(6):1125-1130. DOI: 10.1097/TP.0000000000003212.
[46]IokaT ,KanaiM, KobayashiS, et al. Randomized phase Ⅲ study of gemcitabine, cisplatin plus S-1 versus gemcitabine, cisplatin for advanced biliary tract cancer (KHBO1401-MITSUBA)[J].J Hepatobiliary Pancreat Sci,2023, 30(1): 102-110. DOI: 10.1002/jhbp.1219.
[47]BoradMJ,BaiLY,RichardsD,et al. Silmitasertib plus gemcitabine and cisplatin first-line therapy in locally advanced/metastatic cholangiocarcinoma: a phase 1b/2 study[J]. Hepatology, 2023, 77(3): 760-773. DOI: 10.1002/hep.32804.
[48]KelleyRK,UenoM,YooC,et al. pembrolizumab in combination with gemcitabine and cisplatin compared with gemcitabine and cisplatin alone for patients with advanced biliary tract cancer(KEYNOTE-966): a randomised, double-blind, placebo-controlled, phase 3 trial[J].Lancet,2023,401(10391):1853-1865. DOI: 10.1016/S0140-6736(23)00727-4.
[49]ShiGM, HuangXY, WuD, et al. Toripalimab combined with lenvatinib and GEMOX is a promising regimen as first-line treatment for advanced intrahepatic cholangiocarcinoma: a single-center, single-arm, phase 2 study[J].Signal Transduct Target Ther,2023,8(1):106. DOI: 10.1038/s41392-023-01317-7.
[50]DongX,ZhangZ,ZhangQ,et al. Triple therapy in biliary tract cancers: GemOX plus immune checkpoint inhibitor in combination with lenvatinib or NGS-guided targeted therapy[J].J Cancer Res Clin Oncol,2023,149(5):1917-1927. DOI: 10.1007/s00432-022-04166-z.
[51]HardingJJ, KhalilDN, FabrisL, et al. Rational development of combination therapies for biliary tract cancers[J]. J Hepatol,2023,78(1):217-228. DOI:10.1016/j.jhep.2022.09.004.
[52]ZhengZK,WangJL,LiWX,et al. Anti-programmed cell death protein-1 therapy in intrahepatic cholangiocarcinoma induced type 1 diabetes: a case report and literature review[J]. Front Public Health, 2022, 10: 917679. DOI: 10.3389/fpubh.2022.917679.
[53]HuangQ, WangF, ZhangX,et al. Percutaneous transhepatic cholangial drainage or antibiotic therapy worsens response to immunotherapy in advanced cholangiocarcinoma[J]. BMC Cancer, 2023, 23(1):657. DOI: 10.1186/s12885-023-11128-2.